A warming world: range expansions of lone star ticks, Amblyomma americanum, and the alpha-gal they carry

Female lone star ticks are easily identified by the white or off-white spot on the center of their back.

A trio of trouble (clockwise from top): Blacklegged Tick (vector of Lyme and other diseases), Lone Star Tick (vector of alpha-gal and other diseases), American Dog Tick (vector of Rocky Mountain spotted fever and others).
After clearing some land last week in tick territory, I returned home to find two ticks embedded in my left shoulder. Fortunately, they were easily removed with forceps and having fed for only a few hours, my risk of being infected with a tick-borne illness was exceedingly small. So, with the return of temperatures in the 70s and 80s over the past couple of weeks here in the DMV, reports of ticks attached to humans and pets is on the rise and will continue to increase over the next several months. Let’s dive into the business of climate change and range expansions first. Ticks and insects are cold-blooded, ruthless maybe, but in the biological sense they are largely dependent on ambient temperatures found in their environment to support physiological processes like growth, development, and movement. During winter’s chill in the Washington DC – metropolitan region, with temperatures in the 30-degree Fahrenheit range, it is simply too cold for ticks to move about seeking blood meals from warm-blooded hosts. As temperatures rise in late winter and spring, ticks awakened from their chilly torpor to quest for the blood of animals. Blood provides the protein and other nutrients necessary for ticks to grow, develop, and reproduce. As our world warms, spring’s warmth arrives earlier and autumn’s glow often lasts past Thanksgiving here in the DMV. The lengthening of the warm season provides ticks with more days to be active and to acquire these vital blood meals.
In addition to limiting mobility, cold temperatures can be lethal to ticks just as they are to other forms of life. A very cool laboratory study by Dr. C. S. Burks and colleagues found that 2 hours of direct exposure to temperatures below 7° Fahrenheit proved lethal to lone star tick immatures (nymphs) and adults. Part of this study, conducted in the winter of 1993-1994, also found that these low temperatures did not occur on the forest floors in Ohio, lucky for those ticks back in the day. Leaf litter on the forest floor and snow cover provide insulation for overwintering ticks, enhancing their survival even on very cold nights. The large mass of the earth itself provides a thermal refuge for creatures on the ground and just inches below the soil surface. Nonetheless, lone star ticks have expanded their range further northward over the last seven decades from their historical northern limit of Iowa, Illinois, Ohio, West Virginia, Maryland, Delaware, and New Jersey to historically cooler northern realms including Minnesota, Wisconsin, Michigan, Pennsylvania, New York, Connecticut, Massachusetts, Vermont, New Hampshire, and Maine. This pattern is predicted to continue, or perhaps accelerate as greenhouse gas emissions continue to trap solar energy and warm our planet. A recent study by Dr. R. K. Raghavan and colleagues suggests that future conditions associated with climate change may make maritime regions of Canada climatically suitable for survival of lone star ticks.
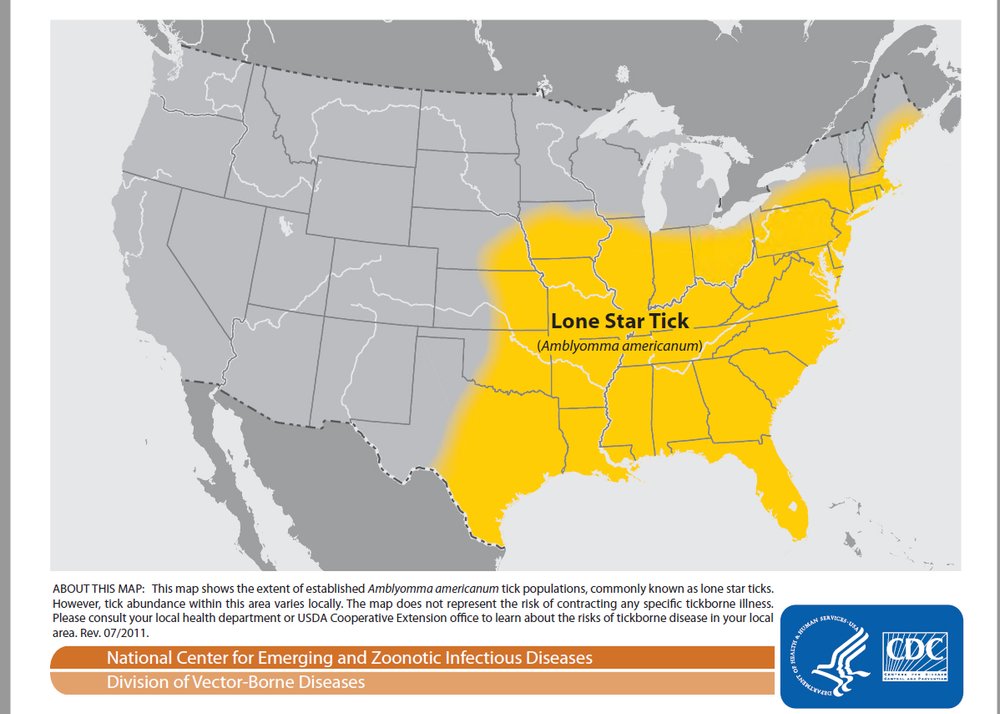
The current range of the lone star tick in the United States has expanded northward in the past century.

Fully engorged ticks are enormous. After feeding for many days, an engorged tick may have increased its body weight 200 times.
Another tick-related story which surfaced last week dealt with folks who had developed an allergy to eating red meat after being bitten by a lone star tick. A friend and colleague developed the red meat allergy known as alpha-gal syndrome after a close encounter with this tick. Let’s dive in and see what this strange sounding syndrome is all about. Alpha-gal syndrome is a human’s immune response to galactose-alpha-1,3-galactose (alpha-gal). Alpha-gal is a carbohydrate molecule found on the surface of muscle cells of many types of wild mammals including mice and rabbits, but also on mammals whose flesh we regularly eat like cattle and pigs. When a lone star tick dines on blood of one of these feral or domesticated animals, it ingests the alpha-gal molecule. When the tick feeds again, maybe on you, it injects saliva laced with alpha-gal. Your body’s powerful immune system recognizes this foreign compound and mounts a potent immune response to it. The immune system produces a library of cells ready to produce antibodies to attack alpha-gal the next time it enters your body. Unfortunately, this may happen when you bite into a juicy burger or pulled-pork sandwich. This second exposure can trigger an allergic reaction that can cause hives, itching, swelling of the lips, face, tongue and throat, wheezing, shortness of breath, runny nose, sneezing, headache, abdominal pain, diarrhea, nausea or vomiting. In severe cases, a person may suffer anaphylaxis, a potentially fatal allergic reaction. Often the reaction does not occur until several hours after the meal. Alpha-gal syndrome is found in many parts of the world including Europe, Asia, and Australia, but it is particularly common in the southeastern United States and now is spreading to other parts of the country. Contracting alpha-gal does not relegate one to a meatless existence. Fish, shellfish, poultry, and other non-mammalian meat sources lack the alpha-gal molecule and may be consumed without fear. A recent study revealed one more piece of disturbing news regarding ticks and alpha-gal. The alpha-gal antigen has also been discovered in the saliva of notorious black-legged ticks implicating them not only as vectors of Lyme disease, but also as potential culprits in the red-meat allergy. Yikes!
Content to chill out on my arm, a female lone star tick makes a mad dash under the probing lens of the camera. Unfed ticks are wafer thin, but after feeding for several days their body weight may increase 200 times. Female ticks convert protein from the blood meal into thousands of eggs.
Reports indicate that the red-meat allergy may decline in time in some individuals. Does the bite of lone star tick mean you are doomed to this allergy? Absolutely not. I have been bitten by lone stars on several occasions and still enjoy a burger now and again with no problem. As with other allergies, individual reactions are complex and may differ from one individual to another. In addition to alpha-gal, lone star ticks transmit several illnesses including Southern Tick Associated Rash Illness (STARI), which has been associated with the bacterium Borrelia lonestari. Symptoms of STARI include a rash, fever, fatigue, and pain in muscles and joints. A second disease spread by the lone star tick is ehrlichiosis. Ehrlichia bacteria produces nasty flu-like symptoms including headache, joint ache, fever, fatigue, muscle ache, confusion, and several other disheartening symptoms.
To reduce the risks of becoming a meal for a tick and the unfortunate recipient of alpha-gal, STARI, ehrlichiosis, or other tick-borne illnesses including Lyme disease, remember the word “AIR”. This stands for avoid, inspect, and remove.
“A” – Avoid ticks and their bites in the following ways. When taking Fido for a walk, stick to the path, trail, or pavement. You are unlikely to encounter ticks on non-grassy surfaces. If you enter habitats where wildlife and ticks are likely to be present, such as grassy meadows, boarders of fields and woodlands, and vegetation along the banks of streams, wear long pants and light-colored clothing. This will help you spot ticks on your clothes as they move up your body. Be a geek – tuck your pant legs into your socks. This forces ticks to move up and over your cloths rather than under them where tasty skin awaits. Apply repellents labeled for use in repelling ticks. Some are applied directly to skin, but others can be applied only to clothing. Don’t forget to treat your footwear, socks, and pant legs. Immature ticks called nymphs are a key vector of diseases and these precautions will help prevent nymphs and adults from attaching to your skin. If repellents are used, be sure to read the label, follow directions carefully, and heed precautions particularly those related to children. If your adventures take you into tick territory, consider placing your cloths directly into a clothes dryer rather than a hamper upon returning home. The heat of the dryer will kill hitchhiking ticks that might otherwise escape clothes in the hamper and cause trouble after your return home.
“I” – Inspect yourself, your family, and your pets thoroughly if you have been in tick habitats. Remember to do this when you return from the outdoors and when taking a shower. A thorough inspection may involve enlisting a helper to view those “hard to see” areas around back.
“R” – Remove ticks promptly if you find them. Removal within the first 24 hours can greatly decrease your risk of contracting a disease. If you find a tick attached, firmly grasp the tick as close to your skin as possible using a pair of fine forceps and slowly, steadily pull the tick out. Cleanse the area with antiseptic. The CDC and the Bug-Guy do not recommend methods of tick removal such as smearing the tick with petroleum jelly or scorching its rear end with a match. Cases of some tick-borne diseases such as Lyme disease are the most common in children and seniors, so take special care to keep kids of all ages safe when they play outdoors.
If you discover a tick that has imbedded in your skin and you wish to determine its identity and discover what disease organisms it might harbor, there are several tick testing services that will identify the tick and perform molecular analysis to determine several important disease agents it may be carrying. On a recent encounter with a tick, after removing a lone star from my waist, I sent it off to a tick-testing laboratory. Within a week, I had results and this little rascal tested negative for the causal agents of Lyme disease, relapsing fever, anaplasmosis, Rocky Mountain spotted fever, Pacific Coast tick fever, tularemia, and ehrlichiosis. Lucky me. If you find an embedded and engorged tick, consider sending it to a tick-testing lab. If it tests positive for one or more tick borne diseases, consult your physician and develop an action plan. Several tick testing services can be found on the internet by simply googling “Tick Testing Services”. They provide step by step directions to prepare your sample for analysis and where to send it. Tick identification is available through the University of Maryland, but this service does not test for disease agents.

Ticks will climb up vegetation and reach out with forelegs to encounter a host. This behavior is called questing.
Around the home, reduce habitat for small mammals that serve as the blood meal for ticks and the source of disease-causing bacteria. Remove piles of brush, unstacked wood, and rubbish that serve as a refuge for rodents and other small mammals. Mow and remove unkempt grasses, weeds, and other vegetation at the edge of the lawn. Mulch beds that border the transition zone between lawn and forest edge. By opening up these areas, raptors and other predators may more easily spot and remove small mammals. Design patios and play areas for children away from forest edges where ticks are more likely to be found. If you follow these precautions, you can greatly reduce the risk of encountering ticks and associated illnesses, while still enjoying the great outdoors.
Acknowledgements
Bug of the Week thanks Bill Gimpel, Kevin Ambrose, and Livia Albeck-Ripka for providing inspiration for this episode. The fascinating articles “Current and Future Distribution of the Lone Star Tick, Amblyomma americanum (L.) (Acari: Ixodidae) in North America” by Ram K. Raghavan,A. Townsend Peterson, Marlon E. Cobos, Roman Ganta, and Des Foley, “ Range Expansion of Tick Disease Vectors in North America: Implications for Spread of Tick-Borne Disease” by Daniel E. Sonenshine, “Population and Evolutionary Genomics of Amblyomma americanum, an Expanding Arthropod Disease Vector” by Javier D. Monzo´n,Elizabeth G. Atkinson, Brenna M. Henn, and Jorge L. Benach, and “The role of direct chilling injury and inoculative freezing in cold tolerance of Amblyomma americanum, Dermacentor variabilis and lxodes scapularis” by C. S. Burks, R. L. Stewart, G. N. Needham, and R. E. Lee, and “Discovery of Alpha-Gal-Containing Antigens in North American Tick Species Believed to Induce Red Meat Allergy” by Gary Crispell, Scott P. Commins, Stephanie A. Archer-Hartman, Shailesh Choudhary, Guha Dharmarajan, Parastoo Azadi and Shahid Karim were used to prepare this episode.
To read more on the Alpha-gal allergy, check out this recent Washington Post article: https://www.yahoo.com/lifestyle/tick-makes-people-allergic-red-171750634.html
For information on Tick Identification in Maryland, click on: https://health.maryland.gov/phpa/OIDEOR/CZVBD/Pages/Tick-Identification.aspx
This post appeared first on Bug of the Week